The science
What is the big idea / how does it work?
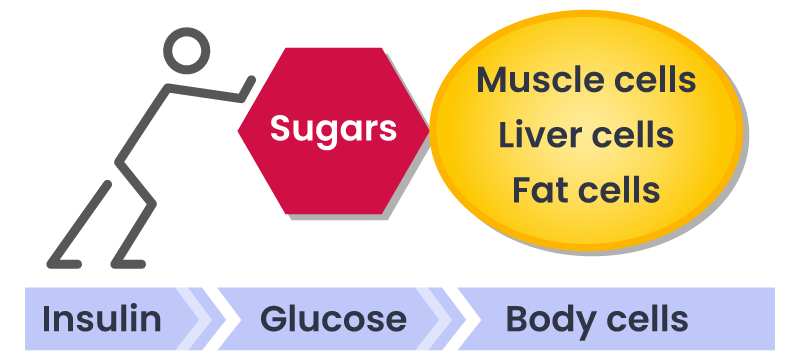
Carbohydrates, (whether from sugars or starches) have a direct influence on blood sugar levels in our body, the more carbs we eat the higher the levels of sugar in our blood. The body regulates blood sugar levels using insulin. If we eat a lot of carbohydrate the body has to produce more and more insulin to cope.
Insulin encourages fat storage, the higher the levels of carbs, the higher the level of insulin, the more fat cells aren’t used for energy but are instead stored as fat.
People who have high insulin levels are in fat storing rather than fat burning mode. It’s often compared to filling a car boot with petrol, where it just sits and stays as it can’t be used to run the car, rather than in the fuel tank where it can be used up running the engine.
Insulin pushes glucose into: muscle cells (energy), abdominal fat, liver and pancreas cells (triglyceride)
Insulin – the key hormone
Background
Interesting fact:
The average adult has about approximately 5 litres / one gallon of blood in their circulation.
Normal blood sugar levels equate to just one teaspoon of sugar within that gallon of blood.
Just imagine the work that your body has to do to deal with the 10 teaspoons of sugar that are contained in a can of Coke. Luckily we have the hormone insulin that helps us deal with this.
Insulin is a hormone produced by the pancreas gland which enables us to store energy as glycogen or fat. It is essential to life. When you eat a meal or a snack, your blood sugar levels go up and your pancreas responds by producing insulin which is circulated in the bloodstream. Your blood insulin levels go up, which signals to the body’s cells take up blood sugar to utilise it or store it as fat.
What happens when there is not enough insulin?
In type 1 diabetes, the cells in the pancreas that produce insulin are damaged or destroyed. Without enough natural insulin, your blood sugar levels would go high, causing a number of complications and potentially coma and death. When insulin became available in injectable form, it transformed the care of type 1 diabetics.
What happens when there is too much insulin?
Type 2 diabetes is a disease that results, largely, from excessive carbohydrate (especially sugar) consumption.
When you eat too many carbohydrates over time, your pancreas has to work really hard, constantly pumping out insulin, to drive your blood sugar levels down to normal levels. As a results, two problems arise:
- Blood insulin levels are persistently high (“hyperinsulinemia”).
- Your body becomes less sensitive to insulin (“insulin resistance”), which means the pancreas needs to make more insulin which drives blood insulin levels up further still, as the pancreas attempts to compensate.
Eventually, your pancreas becomes no longer able to produce any higher levels of insulin and your body becomes resistant to it. Your blood sugar levels start to rise and you develop type 2 diabetes. Medication can help reducing blood sugar levels, but it only papers over the cracks.
As insulin is a fat storage hormone, having persistently elevated blood insulin levels makes it very difficult to lose weight and can make you constantly hungry.
A bit about sugar
Sucrose is the most common sugar found in table sugar, processed food and fizzy drinks. It is made from two molecules – glucose and fructose. Glucose is the sugar that circulates around the body – when we refer to blood sugar, what we are referring to is blood glucose. Fructose does not enter your bloodstream in significant quantities and targets only the liver where it is converted to fat.
So sucrose (glucose and fructose) is particularly unhelpful because:
- Increased blood glucose levels push up insulin (hyperinsulinemia)
- Fructose is quickly turned into liver fat causing “fatty liver” or non-alcoholic fatty liver disease. The liver becomes so overwhelmed by fat that it is no longer able to respond effectively to insulin (insulin resistance).
Hyperinsulinemia (a high blood insulin level) over time has a number of unhealthy consequences, in particular the deposition of visceral fat (fat coating internal organs), which is a major risk factor for developing a number of problems, including heart disease. Fat is also deposited in the pancreas, which further compounds the problem.
Type 2 diabetes is the end point of a very long road of hyperinsulinemia. A large proportion of the population have hyperinsulinemia through excess carbohydrate metabolism, causing visceral fat, long before they’re even pre-diabetic. It is quite possible to have hyperinsulinemia without being overweight. It is estimated that 88% of the U.S.A. population is “metabolically unhealthy” in this way.
The solution?
Cut sugar and starchy carbohydrate consumption. This will reduce blood sugar (glucose) levels. It can also help empty the liver of fat, improving insulin resistance, making you more “insulin-sensitive”.
In 2014, some research was undertaken, (the DIRECT study), which showed that people who followed a rapid weight loss regime based on this low carbohydrate/high fat way of eating not only lost weight fast, but in doing so, cleared fat out of their pancreas and livers and were able to actually put their type 2 Diabetes into remission. A number of the study participants were able to stop their diabetes and blood pressure medication as a result of their weight loss and healthier lifestyle and the majority of them managed to keep the weight off longer term as well.
These results are being reproduced all over the world by patients adopting the low carb lifestyle. We are starting to see many of our own patients improve their diabetic control and we have been able to de-prescribe a number of medications.
